In this section
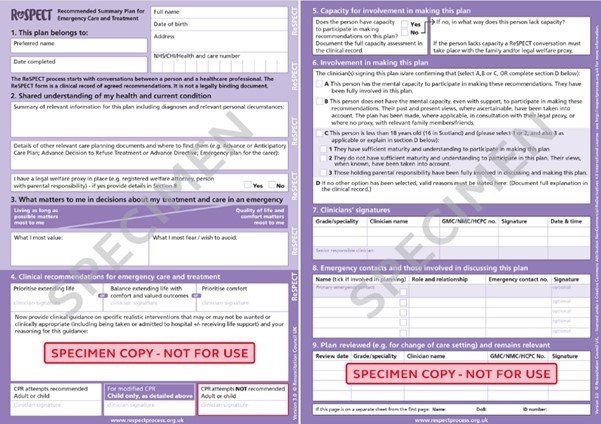
ReSPECT – Recommended Summary Plan for Emergency Care and Treatment
If you suddenly became ill, would anyone know your wishes?
At times of ill health, you may not be well enough to express your wishes to Health Professionals who are caring for you. Planning ahead can help reassure you that decisions about your care and treatment reflect what you would, or would not, want. Letting your family, friends, doctors and nurses know about your wishes, can help them make right decisions for you. This might include treatments you would consider and those you would want to avoid.
Thinking about what would be important to you can ensure plans are put in place to achieve your wishes. This can allow you to be in control even when you are unwell and can also be a comfort to those who care for you. Not everyone will want to have a conversation about their wishes and that is fine.
A ReSPECT form (Recommended Summary Plan for Emergency Care and Treatment) can be used to record your wishes and preferences so that in the event of an emergency, those looking after you can make decisions about your care that reflect your personal wishes.
As part of a ReSPECT discussion, cardio-pulmonary resuscitation (CPR) will be discussed. You can be for CPR and still have a ReSPECT form. However, they are often completed for those patients where CPR is not appropriate, or against their wishes.
For some patients, a decision not to resuscitate may be appropriate or against their wishes and this can be reflected on the form.
You may have heard of a ‘DNACPR statement’ but these are being phased out nationwide and are now being replaced by ReSPECT plans as they allow other important wishes to be recorded alongside a CPR decision.
What is cardiopulmonary resuscitation (CPR)?
If your heart stops beating it may sometimes be possible to start it beating again. Attempts to restart your heart will include pressing down firmly on your chest again and again and breathing for you. In some circumstances, healthcare staff might use a machine to give your heart an electric shock to try to get it to start working again. They may put a tube down your windpipe to help you breathe. They may also give you drugs to help your heart start. This is called cardiopulmonary resuscitation (CPR).
Do people fully recover after CPR?
Each person has a different chance of CPR working. The likelihood of successful CPR is generally determined by the reason your heart stopped in the first place. Overall CPR is not a very successful treatment and only about two out of ten people who have CPR survive and go home from hospital. Survival is less likely in people with lots of health problems, or those who are not close to healthcare professionals at the time their heart stops. Even if CPR does start the heart again, people may need more treatment afterwards, which might be in an intensive care unit although this would not be appropriate everyone. Many never get fully better and suffer from severe mental or physical disabilities.
Making a decision about CPR?
You have the right to refuse CPR, but this decision needs to be recorded as you will not be able to express this at the time you need it because you will be unconscious within seconds of your heart stopping.
Some conditions can make it very unlikely that CPR will help. This applies to a variety of health conditions that many people already live with, even though they feel well enough from day to day.
People who are unlikely to be helped by CPR may be medically advised it is not appropriate. A "not for CPR” statement can be made by certain health professionals if CPR would not help you. The health professional completing the form is obliged to tell you if a ReSPECT plan is made for this reason, unless you say you don’t want to be told.
Every “not for CPR” decision must be weighed up carefully by the health professional, in discussion with the person and/or nominated next of kin. It must be a decision that respects the quality of life the person enjoys, regardless of any disability they currently live with. A ReSPECT plan cannot be made for a group of people: every single person must be considered individually.
Please speak to your doctor or nurse if you would like to talk about this during your admission. If you wish to discuss this once discharged home, please speak to your GP practice or community team.
ReSPECT Form